Over the past ten years there has been a trend toward immersing students into clinical settings earlier at the expense of anatomy laboratory time. This diminishing laboratory time has been abetted by the increasing prominence of remote learning, which, in turn, is compounded significantly by the recent COVID epidemic.
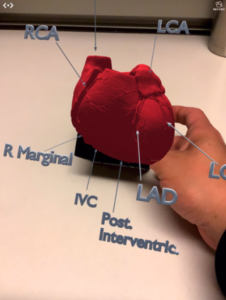
Medical students must now learn anatomy with less opportunities for dissection and lab time and must rely on textbooks, videos, online lectures, and slides which, at best, provide 2D images of complex 3D structures. Augmented reality overcomes these limits on learning by projecting 3D images onto real world backgrounds. Users can interact, for instance, with an anatomical structure by rotating, zooming, and toggling layers on and off while also getting a much better sense of visual and spatial relationships. Users can view these models through head-mounted devices such as Microsoft’s HoloLens or through mobile devices such as an iPad or iPhone in conjunction with a haptic tool such as a Merge Labs’ Merge Cube.
At Sira Medical we’re developing augmented reality software to help clinicians with pre-surgical planning by providing them with patient specific holograms derived from the same data used to generate a conventional CT scan or MRI. Our software enables surgeons to make virtual cuts, simulate corrections, measure bone thickness, take 360° anatomical tours, and size medical implants, among other features.
One other area of great interest for us involves using augmented reality as a teaching tool for medical students. To date, augmented reality has not been extensively studied as an educational intervention or as an alternative to anatomy laboratory learning.
But how effective is augmented reality as a teaching tool relative to learning directly on anatomical specimens? We conducted a study at UCSF involving medical students attending a peer teaching program (PTP). Medical students attend PTP sessions during their first two years of med school. These sessions take place in anatomy laboratories where senior peers review anatomy topics often by leading a demonstration on cadaveric specimens.
We had a pool of 22 students who self-selected into two groups – 17 of the students reviewed an augmented reality cardiac vasculature model above without the benefit of PTP instruction and five reviewed the model after receiving PTP instruction. Augmented reality proved its worth – there was no significant difference in post-intervention testing between the two groups.
Clearly more testing needs to be done and in fact we are about to undertake a second effort at UCSF. But early indications are encouraging and in an environment that is relying less on laboratory time, augmented reality more than fills a critical need.