A child plays high on the monkey bars at the neighborhood playground. Distracted for the slightest moment, she slips and falls, and off she goes to the emergency room. Many of us as parents have been there. If it’s not an elbow fracture, it’s a broken leg, concussion, or worse.
Once in the emergency room the doctors begin imaging to “see” the injury and how best to repair. If the child has a complex fracture for example, an operation is not without risk. Putting bone fragments back in the right place is akin to putting a jigsaw puzzle together and oftentimes many of the fragments fail to show clearly on the imaging requiring surgeons to make critical decisions on the fly during surgery as they encounter these hidden or unexpected pieces of bone.
The risk, of course, is to your child who is on an operating table under an anesthesia mask. Surgeons know if they don’t get their surgery right, there are consequences – malunions, deformities, and surgery re-dos are just a few examples. In fact, these are not isolated incidents. Hidden or unexpected anatomy plays a part in 25% of all surgical errors.
Augmented reality models provide much clearer imaging and significantly reduce the threat of an anatomy surprise. A comparison of a conventional CT scan and an augmented reality model of that same scan is below:
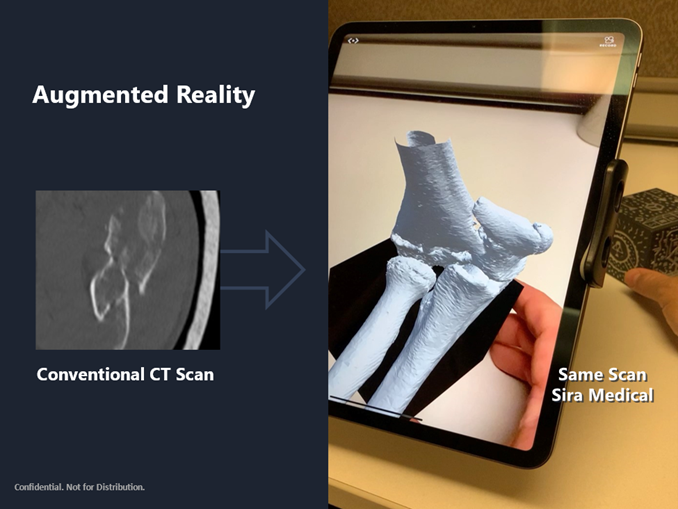
The difference in the imaging is night and day. Surface rendered augmented reality models like the one above, where anatomical layers can be segmented separately and tailored to the surgeon’s needs, also enable surgeons do a number of productive things before stepping into the operating room such as simulating the fracture correction; measuring angles, distances, volume, and bone thickness; and pre-measuring implants such as screws, among other capabilities. The efficiency this brings to the surgeon’s operative plan and into the operating room is material. Pilot studies show measurable time savings. During Sira Medical’s pre-surgical planning pilot study at the University of California, San Francisco, for example, we were estimated to save over 20% of surgical time, not only bringing cost savings opportunities but providing surgeons with more planning confidence and reducing their cognitive load.
Augmented reality models are accurate and precise. Surgeons can take enormous comfort from the fact that the anatomy they see with augmented reality models will be the anatomy they see when they commence surgery. In fact, augmented reality models provide anatomical clarity and fidelity that is difficult to beat.
Augmented reality makes surgeons better at what they do and their lives easier. And for models that can be created in as little as a few minutes, do not change workflows, and are delivered via devices that do not require a steep learning curve, the case for augmented reality replacing conventional imaging is compelling. The future of medical imaging is with augmented reality.